I have written about the challenge of diagnosing lupus in a previous blog. In that post, I described the simplistic checklist that exists for diagnosing this often inscrutable, and potentially life threatening autoimmune disease. Recently, a friend consulted her GP because the possibility of a lupus diagnosis had been suggested in the past. The rheumatological symptoms that suggested this diagnosis had persisted, and had even become more severe.
Arthritis of the Right Hand
Image credit: CDC/Dr. Sellers, Grady Hospital. Used under CC 1.0 Universal public domain license. One of the most common symptoms of lupus is inflammatory arthritis. Although, a patient may have lupus, and also have another type of arthritis.

The GP's response to my friend's query was: what difference would it make if you were diagnosed with lupus? In this blog I will try to explain (to the GP and others) why an accurate diagnosis of lupus is critically important. As a matter of fact, clarity of diagnosis is essential for the delivery of appropriate medical care in any situaiton. This clarity will not only offer the patient efficient and effective treatment for a malady, but almost as importantly, will help to avoid costly and even dangerous inappropriate treatment.
Photosensitivity
Image credit: Walt Fletcher. Used under a CC 4.0 license. Developing a rash after exposure to the sun may be quite common, but it is also one of the symptoms experienced by lupus patients. It is estimated that 2/3 of these patients have a sensitivity to UV light, either from a natural or artificial source. In many cases, exposure to UV may cause an exacerbation of systemic disease.

Differential Diagnosis:
It seems logical and proper for doctors to consider likely diagnostic answers to a clinical puzzle, over unlikely possibilities. As a matter of fact, medical schools train doctors to look for the usual and not the unusual. In medical practice, the way this simple rule of thumb is generally stated: If you hear hoof beats, think horses not zebras.
Deductively arriving at a diagnosis is called a differential diagnosis. In arriving at a differential diagnosis, doctors consider observed/reported symptoms, along with diagnostic tests. With this information they distinguish one disorder from others. A differential diagnosis is essentially an educated guess, based on data.
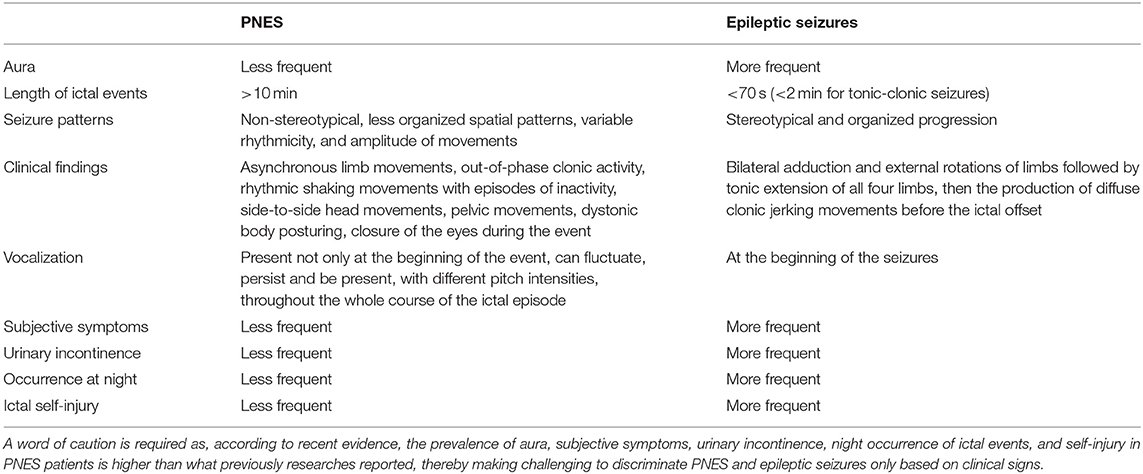
Example of a Differential Diagnosis Chart (Epilepsy)
Image credit: Anzellotti F, Dono F, Evangelista G, Di Pietro M, Carrarini C, Russo M, Ferrante C, Sensi SL and Onofrj M (2020) Psychogenic Non-epileptic Seizures and Pseudo-Refractory Epilepsy, a Management Challenge. Front. Neurol. 11:461. doi: 10.3389/fneur.2020.00461. Used under CC 4.0 license.

If someone does have lupus, and the doctor doesn't know it, the possibility that a zebra (lupus) may be the cause of illness will be disregarded. In such a case, necessary, perhaps essential, treatment will not be administered. When it comes to lupus, the deferral of treatment can be disastrous. If lupus inflammation is central to a problem, or is contributing to a problem, that issue should be treated aggressively.
Lessons From COVID-19 About Catastrophic Inflammation
Most of us have read that long-term effects from COVID-19 may arise from inflammation, rather than from direct action by the virus. A 2021 study published in Science Daily, for example, describes brain damage suffered by COVID-19 patients. Though there is no evidence of virus in the brain, brain damage has occurred. The authors of the article suggest, "neurological changes often seen in these patients may result from inflammation triggered by the virus in other parts of the body or in the brain's blood vessels".

I have read other descriptions of diffuse inflammation from COVID-19. As I read theses descriptions, I thought of the similarity to lupus inflammation. In lupus, a pathogen does not attack organs. Inflammation is the antagonist. An unchecked lupus flare can be, and often is, fatal. As a matter of fact, before the era of effective medication and diagnosis, lupus was considered a progressive, fatal disease. The chances of being alive 5 years after diagnosis was less than 50%.
Synthesizer Used by Musician/Producer J. Dilla, Lupus/TTP Victim

Image credit: Renee Fields. Picture taken at the National Museum of African American History and Culture. Used under CC 3.0 license J. Dilla was a hip hop rapper/producer who died in 2006 after a battle with a rare blood clotting disorder, TTP (thrombocytopenia), a manifestation of lupus.(TTP also occurs in people who don't have lupus)

Thrombocytopenia, Lupus, COVID-19, and Adenoviral COVID-19 Vaccines
The TTP that killed J. Dilla was an inflammatory blood clotting disorder, a rare manifestation of lupus. TTP is also an inflammatory condition associated with COVID-19. An even more interesting fact: TTP, or TTP-like syndrome, is associated with the J&J and Astro-Zeneca vaccines.
There are cases where latent, lupus-associated TTP (such as J. Dilla had) was activated by a COVID-19 infection. In one case, reported by doctors at Keio University School of Medicine, Tokyo, familiarity with the patient's history helped doctors come up quickly with appropriate care. Doctors were able to treat both the COVID-19 infection and the blood disorder successfully. The patient recovered.
In each instance listed above (lupus, COVID-19, and adenoviral vaccines), it is believed activated autoantibodies cause inflammation, which results in diffuse blood clots.

Inflammation Destroys Tissue, and Kills
In discussing TTP, and the inflammatory effects of COVID-19 on brain tissue, I hope to convey the serious nature of unchecked inflammation, no matter the cause. If someone has lupus, it is extremely important for attending physicians to have this information.
Lupus and Infection
Even common infections, which might be inconsequential in most patients, can precipitate inflammation. The physician in that case needs to be able to distinguish symptoms of a lupus flare from symptoms of the infection.
In response to the question of my friend's GP: what difference would a diagnosis of lupus make? The difference can mean avoiding severe organ damage, or even death. Any time someone with lupus is sick, a flare may be precipitated. Any flare should be cut off before it has a chance to escalate.

Finally, wise patients become custodians of their own health. Patients, armed with information about the diagnosis of lupus, are better able to monitor fluctuations of their disease and head off problems before these become significant.
So what did my friend's doctor do in response to the query about lupus? Happily, the doctor seems to have done most of the right things. In addition to the usual blood panel, a bunch of specific tests were run.
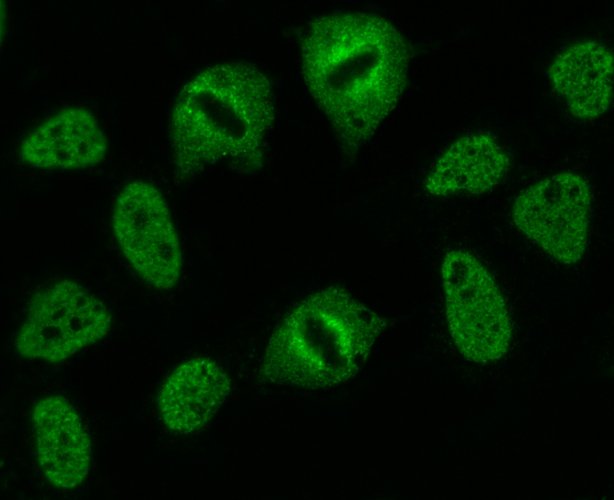
ANA (Anti-nuclear Antibodies), Speckled Pattern)
Image credit: Simon Caulton. Used under a CC 3.0 license. Speckled pattern of ANA is suggestive of certain diseases. It is one of the patterns associated with lupus.

Two tests looked directly for the presence of autoantibodies:
ANA (antinuclear antibodies): these autoantibodies are present in many conditions, and in healthy people. However, they are found in 98% of people who have lupus
Anti-dsDNA (anti-double double stranded DNA): these autoantibodies are found in many conditions, but are considered to be highly suggestive of lupus.
And then the doctor looked for indications that inflammation might be at work, especially if there might be kidney involvement . The National Kidney Foundation suggests that about 90% of people with lupus have kidney inflammation, although actual damage needing treatment may be found in a much smaller number of people. The GFR (kidney filtration rate) (which the doctor asked for) might show that.

A whole bunch of other tests that might indicate general inflammation were run. Also, the doctor ran tests to rule out other diseases (such as rheumatoid arthritis).
What were the results? In all, good news. Everything was negative, except the ANA, which was mildly positive for lupus. My friend was left with an array of rheumatological symptoms and no definitive diagnosis. Lupus remains a possibility, particularly since there are family members who have it, but right now she gets a pass.




Accent pictures (Puzzle, Test Tube, Geometric Design, Microscope): I created them for this blog.
Some Sources Used in Writing This Blog
1.@agmoore/time-to-throw-away-the-diagnostic-criteria-for-systemic-lupus
2.https://www.hss.edu/conditions_managing-arthritis-in-lupus.asp#commonarthritis
3.https://lupus.bmj.com/content/2/1/e000084
4.https://www.nursingcenter.com/ce_articleprint?an=00006205-201404000-00006
5.https://www.hopkinsmedicine.org/news/media/releases/diagnostic_errors_more_common_costly_and_harmful_than_treatment_mistakes
6.https://www.lupus.org/resources/research-on-photosensitivity-among-people-with-lupus
7.https://agribusiness.purdue.edu/consumer_corner/thats-probably-not-a-zebra/
8.https://www.medicalnewstoday.com/articles/differential-diagnosis#definition
9.https://www.jucm.com/wp-content/uploads/2020/12/2006-12-10-15-Clinical-Feature.pdf
10.https://ard.bmj.com/content/78/6/736
11.https://www.sciencedaily.com/releases/2021/04/210416120044.htm
12.https://pubmed.ncbi.nlm.nih.gov/15351310/
13.https://www.rollingstone.com/music/music-news/j-dilla-dead-at-thirty-two-90005/
14.https://onlinelibrary.wiley.com/doi/full/10.1002/1529-0131%28200101%2944%3A1%3C170%3A%3AAID-ANR22%3E3.0.CO%3B2-T
15.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7335418/
16.https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-04-23/03-COVID-Shimabukuro-508.pdf
17.https://www.bmj.com/content/372/bmj.n699/rr-24
18.https://ard.bmj.com/content/80/5/e77
19.https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/lupus-and-infections#diagnosing-an-infection-in-someone-with-lupus
20.https://www.healthline.com/health/blood-tests#routine-tests-and-others
21.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142026/
22.https://www.hopkinslupus.org/lupus-tests/lupus-blood-tests/
23.https://labtestsonline.org/tests/anti-dsdna
24.https://kidneyhi.org/lupus-and-kidney-disease
25.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4635373/
Originally posted here: https://hive.blog/hive-196387/@agmoore/what-difference-would-a-diagnosis-of-lupus-make



No comments:
Post a Comment