Hello everyone... Welcome to my vlog where week after week I share topics of interest from the medical area in which I work as a professional. In this opportunity I am going to show you a medical therapeutic technique for the management of those patients with hyperthermia and whose cause tend to be multiple, and that put in risk the life of the patient in a matter of hours of not being treated by a multiorgan failure, generating a high mortality rate.
Heat stroke patients can usually be difficult to treat even after resuscitation and medical stabilization.
We must first understand that a heatstroke is that pathological entity resulting from overheating suffered by an organism when exposed to high and extreme temperatures or intense physical effort, where the state of hydration and diuresis plays an important role.
Currently, this pathology triggers a high mortality rate worldwide, being observed more frequently in countries with extreme temperature climates, as is the case of the United States where it is estimated that each year approximately 300 people die per year, being one of the most catastrophic events the heat wave that occurred in Chicago in 1995 with a total of 400 deaths and more than 3000 injured as a result of this supernatural event.
Heat stroke is considered a medical emergency and is considered by some to be the most important of environment-related diseases due to its high potential morbidity and mortality.
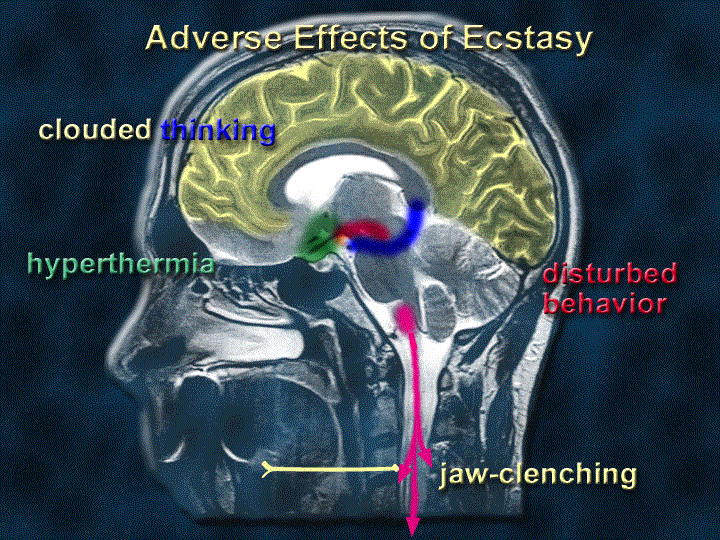
The most effective method of cooling remains a controversial issue. The essential technique is based on quickly recognizing those symptoms and immediate medical intervention and treatment. The ideal is to begin cooling the patient in their pre-hospital environment, removing anything that generates heat, moisturizing the skin (keeping it moist) and fanning it to the emergency room.

Public domain Pxfuel
The cooling measures should be modified to what is evidenced by the decrease in body temperature, in order to avoid hypothermia. We must bear in mind that having a temperature around 39 ºC or 102 ºF we have to decrease the measures of hyperthermia and if we manage to reach these temperature figures in the first 30 minutes increases the survival rate.
Physiopathology
The core body temperature is maintained within well-defined limits, thanks to the balance between heat production and heat elimination.
Muscle and metabolic activity generate heat. Most fevers are responses triggered by some microbial activity, whether called bacteria, parasite or fungus, or in those cases where its aetiology is neoplastic or by abnormalities in the thermoregulatory apparatus.
Heat stroke can appear in previously healthy people, who face great environmental thermal stress.
They can originate in patients with altered homeostatic mechanisms, generating an interruption of the oxidative phosphorylation mechanism, thus the enzymatic systems cease to function, temperature regulation is lost and a significant increase in central body temperature above 42ºC is evident.
The energy deposits decrease as the maximum metabolic demands increase, this produces that the cellular membranes increase their permeability, and therefore the entry of sodium, generating a kind of positive feedback capable of reducing the ATP, based on an increase in the flow of ions, an increase in the rate of depolarization of the membranes and of the neurotransmitter activity and consequently an increase in the production of heat.
All these changes cause the cell membrane to lose its integrity, accelerating heat production, proteins are denatured and cause disseminated necrosis when temperature control mechanisms fail.
Finally, cell damage appears as a product of high temperatures sustained by prolonged heat exposure.
The tissues mainly affected are the vascular endothelium, neuronal tissue, hepatocytes, and nephron.
Heat is dissipated through a combination of radiation, convection, conduction and evaporation.
Radiation is the transfer of heat to an object that is not in direct contact, and is assumed to account for approximately more than 60% of heat loss in cold and temperate environments, this being the primary heat source in these conditions.
Convection is nothing more than the transfer of heat to the circulating gas or fluid, while Conduction is the direct transfer of heat by contact. Finally, evaporation is the conversion of a liquid to gas and is the body's main source of heat loss.
Signs and Symptoms
Heat-triggered pathologies include a broad spectrum of symptoms ranging from localized mild edema to neurological alterations resulting from heat stroke.
Heat edema is limited in hands, feet and ankles. This occurs in the first few days of heat adaptation.
The muscular contractures due to heat usually occur and this is because the patient sweats excessively, for which the body originates a response to the stimulus is thirst, need to drink water, and this is free of sodium, establishing a hyponatremia and therefore contractures.
Heat syncope is frequent, this is explained because the organism exposed to high temperatures generates a vasodilatation response and the consequent hypotension, may even be associated with a hydroelectrolytic imbalance resulting from a state of severe dehydration.
Heat exhaustion is the result of excessive loss of body water, electrolytes, or both. We have to know how to differentiate between heat exhaustion and heat stroke where the latter observes marked neurological commitment.
Other nonspecific symptoms include headache, nausea, vomiting, myalgia, and asthenia.
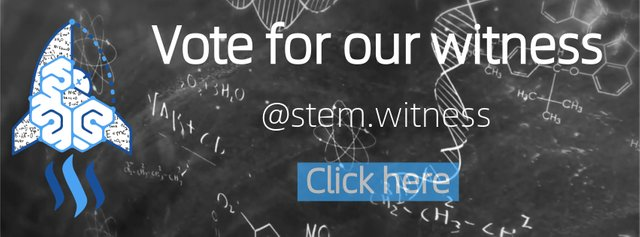
We should suspect heat stroke in any patient who has acute mental state changes or other symptoms of Central Nervous System (CNS) dysfunction in the context of high temperatures and/or history of heat exposure.
Signs of CNS dysfunction may manifest with varying degrees of confusion, delirium, drowsiness, seizures and focal deficits.
Risk Factors
Basic pathologies: autonomic neuropathies, cardiovascular disease, tumours of the Central Nervous System, thyroid storm, pheochromocytoma, diabetes mellitus, among others.
Drugs: anticholinergics, antihistamines, diuretics, lithium, tricyclic antidepressants, among others.
Toxics: amphetamines, cocaine and hallucinogens.
Other situations: thermal suits, extreme temperatures (desert), isolation.
Complications
The main complications of heat stroke are:
Convulsions. Adult respiratory distress syndrome (ARDS). Acute Renal Insufficiency. Hepatic failure. Rhabdomyolysis. Disseminated Intravascular Coagulation.
Indications
Cooling will not harm patients who are hypertensive, regardless of their aetiology. Cooling can save the patient's life after a real heat stroke.
Patient stabilization remains the top priority. We should always initially evaluate the airway, breathing and circulation. Regardless of the need for cooling that helps preserve life should be employed immediately.
Patient Preparation
Immediately remove the patient from the warm environment and remove all clothing.
Stabilize the airway, monitor respiratory pattern and circulation.
The evolution of the patient is closely related to the amount of time the tissues are exposed to the thermal threat.
The cooling rate should not exceed 0.1°C to 2°C per minute, and keep the temperature monitored with a rectal or esophageal thermometer if the patient is intubated.
Techniques
Evaporation
Moisten the patient with cold water. Place large, powerful fans strategically to direct high-flow air currents to the patient's head, feet, and torso.
Spray the patient with water in a spray bottle, in order to keep the individual always moist. Another alternative is to wrap the patient with towels impregnated with cold water and wrap them, repeating this procedure every 5 to 10 minutes.
Stop evaporative cooling when the patient's core body temperature reaches 39°C or 102°F as continuous refrigeration may cause hypothermia, taking into account that body temperature will continue to decrease after evaporative cooling is discontinued.
Always monitor the temperature to make sure it does not rise again. One benefit of this method is that it is very simple and can be used in any emergency room and does not cause any discomfort to a conscious patient.
Immersion in water

Public domain pixabay
Immersion in a cold water bath is a frequent method for the treatment and management of patients with hyperthermia secondary to heat stroke. The patient is immersed for approximately 10 to 40 minutes. Massage the extremities intensely to maintain peripheral circulation and promote heat loss. Frequently monitor body temperature.
Ice

CC0 Public Domain
Initially the use of ice water, an ice pack attached to the body was a very common method used years ago. However, with years of studies and preparation, this method has been criticized even some medical guides do not recommend it, for the fact that the use of ice or ice water can produce a delay in the elimination of heat.
Since ice can generate a vasoconstriction response that generates a blockage in heat exchange, paradoxically the temperature increases and generates unpleasant tremors for the patient.
Treatment
- Channel via the peripheral route, and replace parenteral hydration with 0.9% physiological solution.
- Correct hydroelectrolytic imbalance, secondary to a state of severe dehydration due to losses.
- Quantify diuresis and replenish.
- To monitor vital functions, by means of laboratory monitoring, to request renal function, hepatic, serum electrolytes and gasometry.
- The use of antipyretics may be considered once the temperature reaches or is below 39ºC and based on its etiology.
- Use of anticonvulsants EV, in cases of evidenced convulsive pictures.
- We must never forget the importance of monitoring the temperature during the use of the techniques already described and the vital signs.
- Cooling Rates of Hyperthermic Humans Wearing American Football Uniforms When Cold-Water Immersion Is Delayed. Authors: Kevin C. Miller, PhD, AT, ATC,corresponding author Timothy A. Di Mango, BS, ATC, and Grace E. Katt, BS, ATC. J Athl Train. 2018 Dec; 53(12): 1200–1205.link
- Heat Stroke. SR Mehta and DS Jaswal. Med J Armed Forces India. 2003 Apr; 59(2): 140–143. link
- Physiology, Heat Loss (Convection, Evaporation, Radiation). Lindsey K. Koop; Prasanna Tadi.link
- Oxidative phosphorylation: unique regulatory mechanism and role in metabolic homeostasis. Author: Wilson DFlink
- Physiology, Temperature Regulation. Authors: Eva V. Osilla; Sandeep Sharma.link
- EMS, Methods To Cool A Patient In The Field. Authors: Deena D. Wasserman; Megan Healy.link
- Cooling Techniques For Hyperthermia. Authors: Deena D. Wasserman; Megan Healy.link
- Heat Stroke: Symptoms and Treatmentlink
- Heat syncopelink
- What should you know about hyperthermia?link
- Heat exhaustion. Symptoms & causes. Diagnosis & treatmentlink
- How is heat transferred? Conduction - Convection - Radiationlink
- Heat and Cold. PHYSIOLOGICAL RESPONSES TO THE THERMAL ENVIRONMENT. W. Larry Kenneylink
- Pathophysiology of Heat Illness: Thermoregulation, risk factors, and indicators of aggravation. JMAJ 56(3): 167–173, 2013. Yasufumi MIYAKElink
- Hyperthermia: EMS assessment and managementlink
- Climate change and healthlink
- Dehydration and Heat Strokelink
- Hyperthermialink
- CLINICAL ASPECTS OF INDUCED HYPOTHERMIA METHODS OF PRODUCTION AND INDICATIONS FOR ITS USE BY JOHN W. DUNDEE AND ROBIN KING. Department of Anaesthetics, Queen's University of Belfast, Northern Irelandlink
- Cooling Techniques for Hyperthermia. Updated: May 14, 2018. Author: Erik D Schraga, MD; Chief Editor: Sage W Wiener, MDlink

CC0 Public Domain. Pxhere
Finally, we must monitor the vital signs together with the body temperature, the neurological state of the patient, urine output and correct acid base or hydroelectrolytic alterations which are frequent in these cases.
The use of central venous pressure is useful in these cases. Hypotension is usually common and responds favorably to intravenous solutions and in severe cases that do not respond to parenteral hydration use Dobutamine-type drugs.
Those cases of rhabdomyolysis should be treated aggressively with saline solution, alkalizing the urine, accompanied by an infusion of mannitol in doses of 0.5 per kg of weight plus furosemide if necessary (monitor serum electrolytes).
References

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
I hope you enjoyed my content.
Originally posted here: https://steemit.com/steemstem/@anaestrada12/how-to-treat-a-patie-1575857091


No comments:
Post a Comment