Controlling bleeding from a wound is a priority in the first aid given to every patient, starting from the paramedic who is the first health care worker at a pre-hospital scene until the patient is taken to a specialized care center.
The most frequent injuries observed are those to the extremities, which in some cases become painful due to abundant blood loss. During the Vietnam War, hemorrhages secondary to wounds in the extremities represented the first cause of death in this era.
When dealing with traumatic injuries and trying to provide the best care, medical techniques that allow us to control bleeding quickly and effectively in the first place are essential.

Public domain Pixabay
Physiology of primary hemostasis
The body's protection mechanism against external injuries that generate loss of skin continuity is a phase of primary and secondary hemostasis, where the first phase is mainly mediated by platelets and the second stage of hemostasis will be through coagulation factors, however on this occasion we will describe the first phase for study.
Primary haemostasis is the main biological response to external skin injury, favouring the formation of haemostatic platelet plugs within seconds of a traumatic continuity solution in the skin. Fibrin fibres gather around the platelet plug within minutes. This fibrin network is part of an early response that initiates the wound healing process.
Bleeding control is necessary to establish and provide hemodynamic stability for the patient and to avoid severe compaction and even death.
Hemostasis is the first step in preparing the wound closure and when it does not occur properly or fails, it can trigger hematoma formation, deficit in healing, increase the risk of local and in severe cases disseminated infections, as well as lead to tissue ischemia and death of the affected limb.
Large bruises can cause a dehiscence of sutures in a wound. Bleeding from wounds will depend on the magnitude and depth of the wound, i.e. it may be superficial or deep. Superficial wounds such as abrasions, avulsions or simple lacerations imply damage to the epidermis, dermis and subcutaneous tissue, therefore the bleeding that originates from this type of injury comes from capillaries, small veins or arterioles and therefore the amount of bleeding is usually scarce.
While deep wounds involving the fascia are therefore large vessels and are usually the result of deep puncture wounds, gunshot wounds or major crushing trauma, they mostly trigger exaggerated bleeding.
Therefore how to treat these bleeding wounds will depend on the nature of the bleeding (whether the small or large vessels are affected) the location of the injury and duration with other major organs.
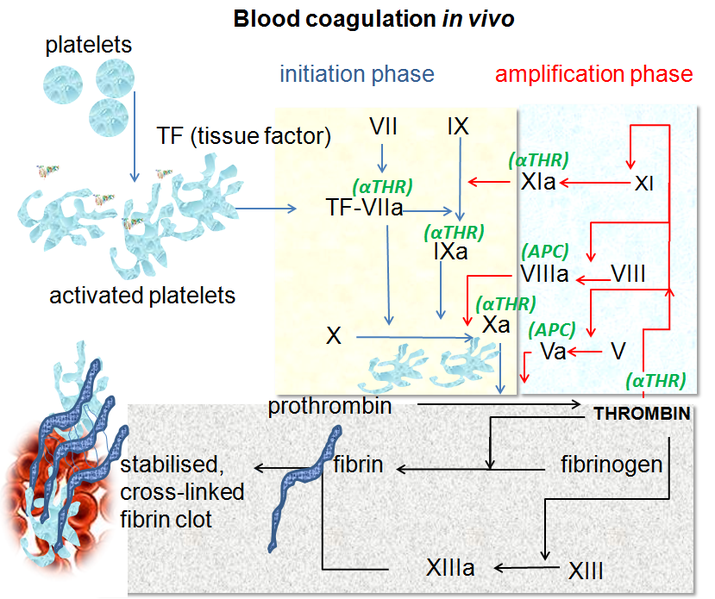
Blood coagulation pathways in vivo. Public domain CC BY-SA 3.0 form Wikipedia
Indications
Immediate control of excess bleeding is always a priority and should be done at the first patient-medical assistant (paramedic) contact. The timing and techniques used to isolate and control the source of bleeding will depend on the priority of treatment for each patient. For example, in a polytraumatized patient, a tourniquet or compression dressing should be applied as the first step in controlling the bleeding.
Contraindications
There is no absolute contraindication to any particular technique that controls bleeding. Every physician should choose the technique best suited to the patient's particular situation. We should never distract attention from a more impressive wound or lose sight of smaller, less conspicuous wounds as these can become life-threatening.
When we are faced with multiple wounds we should use those techniques that are simpler, easier and more effective to achieve control of the bleeding.
Medical Techniques
One of the most important things in controlling bleeding is primary care and management at the point of first contact with the patient. The simplest and most beneficial thing is the execution of direct pressure on the place where the bleeding comes from.
We must consider that those small wounds without hemodynamic involvement could be given a local anesthetic before starting the wound manipulation. It has always been recommended to irrigate contaminated wounds with physiological solution in order to clean them, remove foreign bodies or dirt.
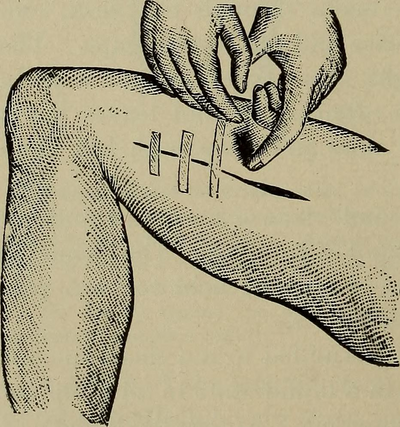
Direct Pressure
The quickest and easiest way to stop bleeding is to apply direct pressure to the bleeding wound. The development of a compression dressing has been useful for many years in controlling bleeding. However, most compression dressings do not exert the correct pressure, allowing them to act as a sponge instead of a compression dressing as such, since what they do is hide blood loss with abundant dressing material.
As soon as possible, the wound(s) should be explored. It is recommended that this be done in a place with good lighting, and circumstances that allow it, since even the most active bleeding can originate from several sources.
The development of direct pressure on the affected blood vessels provides sufficient time to allow the platelet plug to form, thus acting on the natural mechanisms of primary haemostasis. Most injuries are usually controlled within 10 to 15 minutes of pressure being applied to the blood vessel.
The application of pressure on the proximal end of the artery near the injury, prevents the entry of blood and favors the control of bleeding when it is difficult to perform the exploration of the wound in the area of the accident, and should be channeled immediately to a specialized medical center for proper exploration of the wound and its resolution.
Tourniquets
This method has been of great attention and use throughout history, since in reality they are not very useful and beneficial, having better results the compressive bandage, since this last one generates less tissue ischemia, especially in those important wounds by crushing, amputations among others.
The tourniquets can be necessary and useful in disasters in patients with significant bleeding, where controlling the bleeding quickly is the priority and thus gain more time and devote more people injured, the application of this method should be considered as a last resort when other techniques have failed and the patient's life is in danger.
Ligation of the vessels
Active bleeding wounds should be carefully inspected for this method. Initially place a blood pressure cuff near the wound and insulate it until a dry field is achieved. As the cuff slowly deflates, pressure is lost, so the arteries will be the first to show. For effective control, the large and intermediate size vessels should be ligated primarily, but the anatomy of the affected area should be known, especially the extremities that are most frequently affected.
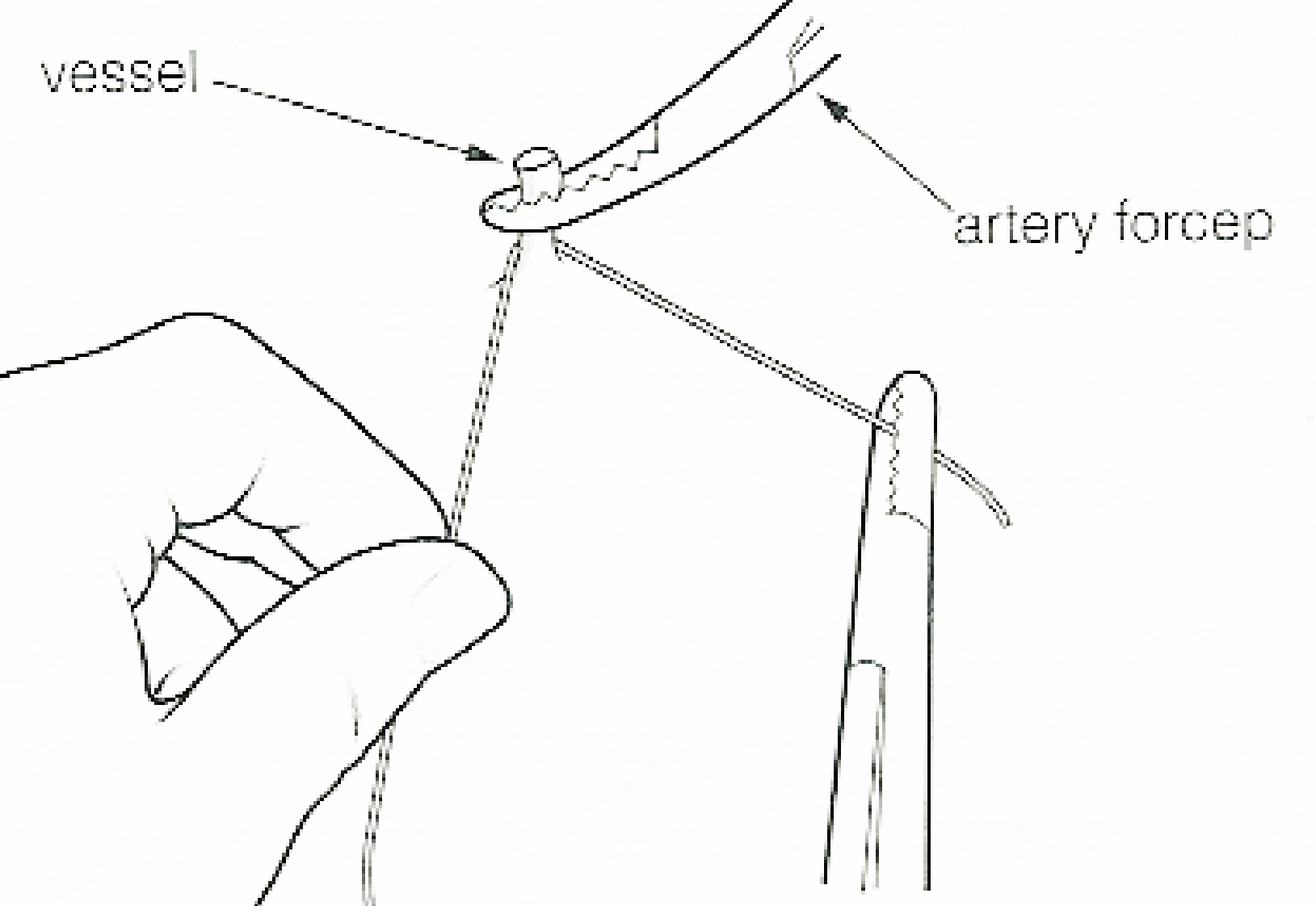
ligature (surgery). Public domain Wikipedia CC BY-SA
The bleeding vessels that are visualized with sutures must be ligated, take the end of the bleeding vessel with a haemostatic forceps, proceed to pass a thread of the correct size and preferably absorbable sutures, finally tie and fix the suture around the base of the bleeding vessel and carefully remove the bleeding forceps.
The Vasoconstrictors
Usually, the small bleeding vessels constrict and will stop bleeding once the large vessels have been treated. Otherwise, it is effective to use local vasoconstricting drugs, such as adrenaline, which can be used in two ways. Applied in the form of an injection around the edges of the wound is often accompanied by local anesthetics, another option is to take a gauze soaked in saline and adrenaline to cover the wound for about 5 minutes.
Alternatively, topical cocaine (1% to 4%) is a potent vasoconstrictor especially in the mucosa. Also used are combinations of tetracaine 0.5%, adrenaline 1:2,000 and cocaine with an anaesthetic effect and for haemostasis of wounds, by means of occlusive dressings on the lesions.
Topical haemostatic agents
Diffuse blood loss sometimes persists after ligation of the most conspicuous blood vessels, even though most of them do not cause hemodynamic involvement, they can trigger problems at the time of wound closure and even aesthetic problems.
The application of oxidised cellulose (Gurgicel) or dry gelatine (Gelfoam) provides a matrix that facilitates the platelets' haemostasis process. The most problematic wounds can be treated with these agents and covered with a pressure dressing, after a few minutes they can be sutured, another option is to leave the haemostatic agent in the wound, close the wound and place a pressure dressing.
Scalp injuries
Public domain from Flickr
Control of scalp bleeding in a polytrauma patient can lead to heavy bleeding and sometimes even hemodynamic compromise. They should be treated and resolved as soon as possible, an alternative is the application of Raney's scalp clips, another option is to place haemostatic clips on the active bleeding points to proceed with the administration of local anaesthesia around the wound and proceed to the realization of eight-shaped stitches, simple continuous sutures or mattress sutures for wound closure.
And finally we have;
Bone exposed wounds
The exposed bone is a bulky wound with a tendency to bleed, which sometimes results in amputations. Bone wax can serve to plug these sites and temporarily stop the bleeding until its final resolution can be executed.
Conclusions
A healthy wound is proof of adequate hemostasis. Routine wound care should include checking a healthy incision line and the absence of bruising or infection.
All the techniques already described in this article, when performed correctly as described, will result in favourable outcomes with a low complication rate. There is a risk of ischemia and loss of a limb each time a tourniquet is used, when this is used for prolonged use, so far it is recommended to use a tourniquet for a maximum of 30 minutes, the tourniquet should be released and evaluated periodically until the resolution of the wound.
Adrenaline or any other type of vasoconstrictor should not be used on the fingers, toes, ears, nose or penis as it may cause ischemia and tissue loss. Care should always be taken when using topical vasoconstrictors so that the total dose administered does not produce adverse effects such as hypertension, tachycardia or convulsions.
Sources:
- Emergency Medical Services. Olive C. Kobusingye, Adnan A. Hyder, David Bishai, Manjul Joshipura, Eduardo Romero Hicks, and Charles Mock.link
- Lessons of War: Combat-related Injury Infections during the Vietnam War and Operation Iraqi and Enduring Freedom. Dana M. Blyth, Heather C. Yun, David R. Tribble, and Clinton K. Murraylink
- Hemorrhage Control. Eric R. Donley; Joshua W. Loyd.link
- Physiology, Clotting Mechanism. Cyrus Garmo; Bracken Burns.link
- Mechanism Action of Platelets and Crucial Blood Coagulation Pathways in Hemostasis. Mercy Halleluyah Periayah, Ahmad Sukari Halim, and Arman Zaharil Mat Saadlink
- Hemorrhagic complications in dermatologic surgery. Christopher G. Bunick and Sumaira Z. Aasilink
- Tourniquet use in the civilian prehospital setting. C Lee and K M Porter, T J Hodgettslink
- Nancy Caroline's Emergency Care in the Streets wrinting for Nancy Caroline, American Academy of Orthopaedic Surgeonslink
- Emergency and Trauma Care for Nurses and Paramedics wrting for Kate Curtis, Clair Ramsden, Ramon Z. Shaban, Margaret Fry, Julie Considinelink
- Primary hemostasislink
- Acute wound carelink
- Cuts and puncture woundslink
- Hemorrhage Controllink
- Wound Foreign Body Removal. Updated: Oct 17, 2019 . Author: Christian C Bannerman, MD, FAAEM; Chief Editor: Erik D Schraglink

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
I hope you enjoyed my content.
Originally posted here: https://steemit.com/steemstem/@anaestrada12/what-should-we-do-wh-1577061258




No comments:
Post a Comment