https://files.peakd.com/file/peakd-hive/agmoore/dWSCwRb1-Qing20Dynasty_Cixi_Imperial_Dowager_Empress_of_China_On_Throne_Sedan_With_Palace_Enuches.jpg
***Dowager Empress of China, Qing Dynasty***

*Image credit: Unknown author, "before 1908". [Public domain](https://commons.wikimedia.org/wiki/File:The_Qing_Dynasty_Cixi_Imperial_Dowager_Empress_of_China_On_Throne_Sedan_With_Palace_Enuches.PNG)* The picture shows the Dowager Empress with her court retinue.

We like to think we are unique, that there is no one like us in the world. However, when it comes to medical care, the law of averages prevails. Unless we are a Donald Trump, a Boris Johnson, or the Empress Dowager of China, we are not likely to receive the highly specialized, tailored treatments that may make the difference living or dying. (Check out quotes at the end of this blog from Johnson and Trump about the exquisite attention they enjoyed when they were stricken with COVID-19.) ***The Law of Averages: Think Horses, Not Zebras***
There's an informal rule medical students are taught to help guide them in clinical practice: ['If you hear hoof beats, think horses, not zebras'.](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6033608/) In other words, the usual, not the exotic, is the first, best place to look for answers. That's the law of averages. When we enter a doctor's office, it is the law of averages that will govern the standard of care we receive. In order for the standard to have utility, doctors must be in command of diagnostic metrics. One of these metrics is [blood pressure.](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4745997/) Another is [gait.](https://medicalxpress.com/news/2018-11-fast-lot-health.html) And, a third, very significant metric, is BMI: [Body Mass Index.](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469873/) ***Gait Can Be Revealing***
“A really strong predictor of mortality is gait speed": University of [Southern California,Health Science Community News](https://hscnews.usc.edu/how-fast-you-walk-says-a-lot-about-your-health)

BMI is admittedly a crude instrument. It was first formulated by [Lambert Adolphe Jacques Quetelet](https://www.npr.org/templates/story/story.php?storyId=106268439) in 1820. However, this seemingly antiquated metric has held up over the years and today has proven to have significant prognostic value. There are conditions in which BMI status correlates, at least approximately, with the likelihood of disease progression. One of these conditions, diabetes, has long been associated with obesity. A more recently recognized condition, COVID-19, has been associated generally with obesity. As a matter of fact, recent studies have shown a remarkably specific relationship between being BMI and severe COVID-19.

###
[The Limitations of BMI](https://www.npr.org/templates/story/story.php?storyId=106268439)
An argument against using BMI as a prognostic tool has been made by critics over the last two hundred years. Even Lambert Quetelet, who formulated BMI, [never claimed](https://www.npr.org/templates/story/story.php?storyId=106268439) it could measure the amount of fat in an individual. He thought the measurement could be used to track rates of obesity in the population as a whole, and therefore be helpful in the allocation of resources.

***Lambert Adolphe Jacques Quetelet***

*Image credit:Joseph-Arnold Demannez (1826-1902). [Public domain.](https://commons.wikimedia.org/wiki/File:Adolphe_Qu%C3%A9telet_by_Joseph-Arnold_Demannez.jpg)* Quetelet was an astronomer, mathematician, sociologist and statistician. He was not a doctor.

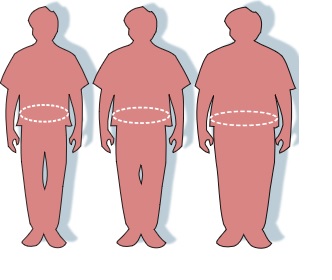
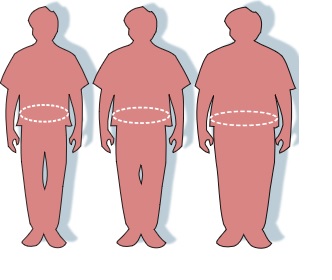
In recent years, the accuracy of BMI in assessing the likelihood of disease process has been challenged by a number of researchers. A 2020 article in [*Nature Reviews: Endocrinology*,](https://www.nature.com/articles/s41574-019-0310-7) for example, asserts that BMI should never be used in isolation but should instead be considered along with another measure: waist circumference. The authors of this article conclude: " the combination of BMI and waist circumference can identify the highest-risk phenotype of obesity far better than either measure alone". ***BMI and Waist Circumference in Diabetes Prognosis*** *
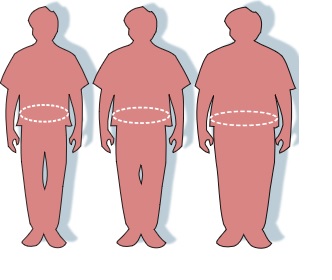
Image credit": Renée Gordon (FDA), Victovoi [Public domain](https://commons.wikimedia.org/wiki/File:Obesity-waist_circumference.svg)* ***Waist Circumference, Visceral Fat and Diabetes*** The importance of waist circumference is that it more accurately indicates the existence of visceral fat, the kind of fat that [wraps itself around organs](https://www.diabetes.co.uk/body/visceral-fat.html) (and directly damages them) than BMI does alone. However, though there is an association between waist circumference and visceral fat, there is no way to tell how much of the fat a person is carrying is visceral and how much is [subcutaneous.](https://paleoleap.com/the-protective-role-of-subcutaneous-fat-and-what-that-means-for-fat-weight-loss/) The only way to tell is to visualize the fat on a scan. Some individuals have a large waist circumference but are [metabolically healthy.](https://www.jci.org/articles/view/129186) They don't have a lot of visceral fat. Conversely, there are lean people who do [store visceral fat.](https://www.theguardian.com/science/2006/dec/10/medicineandhealth.health) Unfortunately, most doctors will not offer patients a scan to determine the amount of visceral fat. Usually, doctors don't even offer a tape measure to determine waist circumference. For most patients, a simple scale will be the standard of care. Law of averages. The challenge doctors face in assessing obesity and predicting its health consequences, is further complicated by ethnicity and race. The authors of an article published in [*Obesity Review*](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968570/) state, "BMI-adiposity relations appear to vary significantly across race/ethnic groups".

It's obvious that the simple formula worked out by Quitelet for establishing BMI is not sufficient in itself for establishing either obesity, or the risk of developing disease. At least one other measure, waist circumference, should certainly be added. For greater certainty, an assessment (by imaging) of visceral fat would give a more accurate picture. However, most of us do not have the resources of Donald Trump, Boris Johnson or the Empress Dowager, so we will likely have to dispense with the imaging. We do not, though, have to dispense with the combined BMI and waist circumference as a rough guestimate of our diabetes risk. These two tools are inexpensive, accessible, and easy to use in a doctor's office (or at home!).
### COVID-19: BMI as a Risk Factors for Severe Outcome Although research suggests limited utility in using BMI to assess the general health risks of overweight/obesity status, there is a growing body of evidence that suggests this simple metric may have significance in predicting COVID-19 outcomes. An article published in [*Diabetes & Metabolic Syndrome: Clinical Research & Reviews*](https://www.sciencedirect.com/science/article/pii/S1871402120302307) reports:

"BMI is strongly linked to risk for SARS-CoV-2 in hospital and COVID-19-related death among UK Biobank participants".

"These associations were stronger for individuals under 70 versus those over 70 years of age at time of pandemic".
 "They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)
"They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)
, compared with whites". One interesting finding in this study (which looked at 4855 participants) was that not only did fatalities correlate positively with higher BMI, but so did test positivity rates. And, these associations were more pronounced in younger people (under 70).


Another study which looked at the relationship between BMI and COVID-19 outcomes was published in the journal [*Obesity Research & Clinical Practice*.](https://www.journals.elsevier.com/obesity-research-and-clinical-practice) This study looked at 6577 critically ill patients admitted to the ICU. One interesting finding in this study was that "Invasive mechanical ventilation was associated with severe obesity and was *independent of age, sex, diabetes, and hypertension*." The authors of the article suggest that obese patients have impaired innate immunity because of the higher percentage of visceral and subcutaneous fat. This extra fat tissue produces "higher concentration of several pro-inflammatory cytokines such as alpha-TNF, MCP-1, and IL-6."


***Sir Richard Quain: Explained Fatty Disease of the Heart, 1850***

*Image credit: Leslie Ward (1851-1922. [Public domain](https://commons.wikimedia.org/wiki/File:Sir_Richard_Quain.jpg)* This caricature appeared in *Vanity Fair* magazine, 1883. Today we know fat around the heart is closely associated with [atrial fibrillation.](https://www.sciencedaily.com/releases/2014/11/141117162618.htm)


The takeaway from the *Obesity Research & Clinical Practice* article is that elevated BMI (≥ 35 kg/m2) is in itself a risk factor for severe COVID-19, and for death from the disease. The authors conclude that patients classified as obese by their BMI are at risk for sever COVID-19, " independent of age, race, sex, and comorbidities such as diabetes, hypertension, dyslipidemia, or pulmonary disease." Finally, an article published on September 28, 2020 in [Diabetes Metabolic Syndrome](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7521380/) describes a meta analysis of studies from across the globe. These looked at the relationship between BMI and COVID-19 outcomes. With a broad population spectrum to consider, the authors find that elevated (greater than 35) BMI correlates significantly with severe COVID-19 disease. In their concluding statement, the authors of this meta analysis state: "BMI should always be assessed in all COVID-19 patients and special attention should be given to patients with obesity."

### Conclusion I began this blog by writing about the law of averages. When the average person receives medical care, treatment will by guided by averages, by what has happened to other people in similar circumstances. BMI is a metric based on averages. Is it useless? Not useless, but of limited utility in some circumstances. However, in other circumstances, such as a COVID-19 infection, BMI can warn care providers about special risks that may exist.

### End Note on Boris Johnson and Donald Trump ***Boris Johnson:*** He [listed](https://www.chicagotribune.com/coronavirus/ct-nw-boris-johnson-coronavirus-20200412-l5iyf2jqprgaxdxfsnhsmwh6je-story.html) a number of the front line staff who cared for him during his week-long stay at St. Thomas’ Hospital in London but singled out two nurses who stood by his bedside for 48 hours “...when things could have gone either way.” And he added, “Because for every second of the night they were watching and they were thinking and they were caring and making the interventions I needed." >*Note from me: While I respect and admire healthcare workers--nurses especially--there simple are not the resources to have two nurses stand at the bedside of every COVID-19 patient who is gravely ill in the hospital.*

***Donald Trump:*** He [told](https://www.newsweek.com/trump-says-great-thing-about-being-president-abundance-doctors-when-you-catch-covid-1538900) the Pennsylvania crowd that top-notch medical care was a benefit of being the president: "If you're not feeling 100 percent, you have more doctors than you thought existed in the world," Trump said. And he added, "I was surrounded by like 14 of them." >*Note from me:* *I repeat, while doctors and nurses are heroic in treating COVID-19 patients--with a dedication that sometimes costs them their lives--there will not be 14 doctors standing around my bed or your bed if we are stricken with this disease.*

*Thank you for reading my blog*

*Hive on!*

### Some Sources Used in Writing This Blog 1.[The thoracic and Cardiovascular Surgeon Reports](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6033608/) 2.[Circulation Research](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4745997/) 3.[Medical Express](https://medicalxpress.com/news/2018-11-fast-lot-health.html) 4.[Social Theory and Health](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469873/) 5.[University of Southern California HSC: News](https://hscnews.usc.edu/how-fast-you-walk-says-a-lot-about-your-health) 6.[NPR](https://www.npr.org/templates/story/story.php?storyId=106268439) 7.[Nature Reviews: Endocrinology](https://www.nature.com/articles/s41574-019-0310-7) 8.[Diabetes.co.UK](https://www.diabetes.co.uk/body/visceral-fat.html) 9.[PaleoLeap](https://paleoleap.com/the-protective-role-of-subcutaneous-fat-and-what-that-means-for-fat-weight-loss/) 10.[The Journal of Clinical Investigation](https://www.jci.org/articles/view/129186) 11.[The Guardian: Medicine and Health](https://www.theguardian.com/science/2006/dec/10/medicineandhealth.health) 12.[Obesity Review](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968570/) 13.[Diabetes & Metabolic Syndrome: Clinical Research & Reviews](https://www.sciencedirect.com/science/article/pii/S1871402120302307) 14.[Obesity Research & Clinical Practice](https://www.journals.elsevier.com/obesity-research-and-clinical-practice) 15.[Science Daily](https://www.sciencedaily.com/releases/2014/11/141117162618.htm) 16.[Diabetes Metabolic Syndrome](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7521380/) 17.[Chicago Tribune](https://www.chicagotribune.com/coronavirus/ct-nw-boris-johnson-coronavirus-20200412-l5iyf2jqprgaxdxfsnhsmwh6je-story.html) 18.[Newsweek](https://www.newsweek.com/trump-says-great-thing-about-being-president-abundance-doctors-when-you-catch-covid-1538900) 19.[CDC](https://www.cdc.gov/obesity/data/obesity-and-covid-19.html) 20.[Science Magazine](https://www.sciencemag.org/news/2020/09/why-covid-19-more-deadly-people-obesity-even-if-theyre-young) 21.[JAMA](https://jamanetwork.com/journals/jama/fullarticle/2772071) 22.[Escardio.org](https://www.escardio.org/The-ESC/Press-Office/Press-releases/Body-mass-index-is-a-more-powerful-risk-factor-for-diabetes-than-genetics) 23.[AHA Journals](https://www.ahajournals.org/doi/abs/10.1161/CIRCRESAHA.120.316101) 24.[Science Direct](https://www.sciencedirect.com/science/article/abs/pii/S016882272030615X) 25.[Psychology Today](https://www.psychologytoday.com/us/blog/the-gravity-weight/201603/adolphe-quetelet-and-the-evolution-body-mass-index-bmi) ### Illustrations Not Already Credited zebra https://pixabay.com/de/vectors/zebra-tier-tierwelt-pferde-152604/ zebra2 https://pixabay.com/de/illustrations/zebra-tier-m%C3%A4hne-streifen-afrika-4864906/ zebra3 https://pixabay.com/de/vectors/afrika-tier-gestreift-streifen-2027038/ Zombie https://pixabay.com/de/vectors/zombie-untote-monster-frankenstein-156055/ scale https://pixabay.com/de/photos/personenwaage-waage-gewicht-1149263/ notation https://pixabay.com/de/illustrations/buchstaben-alphabet-sonderzeichen-659366/ measuring tape https://pixabay.com/de/vectors/ma%C3%9Fband-messung-zoll-metrisch-29455/

Originally posted here: https://hive.blog/hive-196387/@agmoore/the-long-history-of-bmi-new-relevance-with-covid-19










 "They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)
"They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)






















 "They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)
"They were also stronger for non-whites (predominantly South Asians and Afro-Caribbeans)












No comments:
Post a Comment