Hemorrhages are classified according to their location and underlying vascular pathology. In the article below, it will allow us to describe the clinical characteristics and behavior in neuroimaging studies of intracranial lesions called intraparenchymal hemorrhage.
This type of pathology is located, or is part of a complex of brain lesions called intracranial hemorrhage, which are observed in specialized studies such as cranial tomography during the immediate evaluation of a stroke.

The brain. Public domain image source flickr
Irrigation of the brain
The richly vascularized brain constituted by:
The anterior circulation, given by the internal carotid artery which originates from the bifurcation of the Primitive Carotid Artery.
The posterior circulation, occurs through the basilar vertebro system.
These come together and give what is called the Willis Polygon; in the form of a central ring formed by the two internal Carotid arteries, the Anterior Cerebral Artery, a Anterior Communicating Artery and two Posterior Arteries, the Basilar Artery and two segments of the Posterior Cerebral Artery.
Causes of intracranial hemorrhage
The location of the hemorrhage reduces the number of differential diagnoses to a few entities. Below we will develop the causes of intracranial hemorrhages according to their location:
- Causes cranial trauma, location of the Intraparenchymal lesion: frontal lobes, anterior part of the temporal and subarachnoid lobes. They are usually produced by blow and kickback injuries during brain deceleration.
- Cause Hypertensive hemorrhage, location of the Putamen lesion, pale globe, thalamus, cerebellar hemisphere and protuberance. Product of uncontrolled chronic hypertension.
- Causes ischemic cerebrovascular, event with hemorrhagic transformation. Location of the lesion Basal ganglia, subcortical and lobular regions.
- Cause Metastatic tumor, location of the Lobular lesion. They tend to be lung lesions, choriocarcinoma, melanoma, renal cell carcinoma, thyroid, and atrial myxoma.
- Cause coagulopathies, location of the lesion any area of the brain. They are rare, usually associated with stroke.
-
- Cause Drugs or drugs, location of the lobular, subarachnoid lesion. It is associated with the consumption of Cocaine, amphetamines, and phenylpropranolamine.
- Cause Arteriovenous malformation, location of the Lobular, intraventricular and subarachnoid lesion.
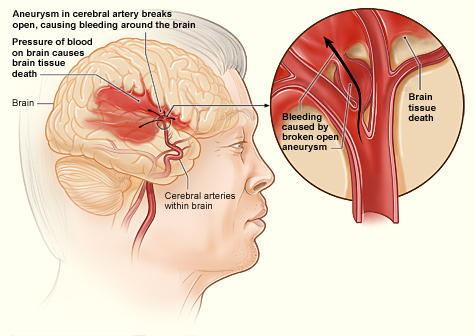
- Cause of aneurysm, location of the Subarachnoid lesion, intraparenchymal, rarely subdural.
Important note: Much of the information provided in this section is very similar to different pages and books found on the web, because this information type can not be modified, since the alteration of the information can be confusing.
Intraparenchymal hemorrhage
Fomra part of intracranial hemorrhages, is one of the most frequent of all previously cited. It represents approximately 10% of the strokes and its mortality rate is 50%. With higher rate of incidence in dark race and whose cause is the presence of high blood pressure values, (arterial hypertension) or traumatic brain injury.
There are risk factors that predispose the appearance of these cerebrovascular events as it is; old age and rampant alcoholism.
On the other hand, the diagnosis of this pathology in young patients is associated with the consumption of illicit substances such as cocaine.

Alcoholism. Public domain image licensed CC BY-SA 4.0
Intraparenchymal haemorrhage of hypertensive origin
Hypertensive parenchymal hemorrhage, also known as hypertensive hypertensive or intracerebral hemorrhage, arises as a result of spontaneous rupture of a small artery located deep in the brain.
The most frequent locations are: the basal ganglia (the putamen, the thalamus and the adjacent deep white substance), the deep part of the cerebellum and the protuberance.
It is important to bear in mind that when this hemorrhage occurs in an individual without a history of hypertension and apparently healthy, it is essential to rule out the presence of coagulation disorders, neoplasms, vascular malformations among others.
Apparently, the small arteries of the mentioned regions are the most prone to injury because of malignant hypertension. Sometimes the hemorrhage is usually small, scarce while others form a large clot that compresses the adjacent tissue, causing brain herniation and death.
When the blood volume lost through one of these arteries, the blood can reach penetrates the ventricular system, which would increase the risk of morbidity, and even cause a secondary hydrocephalus.
Once the event occurs, only 48 hours are enough for the body to find a way to correct this alteration and that is why they begin to produce and release macrophages which are responsible for phagocytosis the outer surface of the hemorrhage.
At the beginning of this process guided by the macrophage, after one to six months, the hemorrhage has usually disappeared and has turned into an orange crack-shaped cavity, covered by glial scar tissue and hemosiderin-laden macrophages.
Clinical manifestations
Intracerebral hemorrhages do not have a direct relationship with physical exercise, but almost always manifest when the patient is awake and, sometimes, when they are under some tension.
The clinical detonating manifestation is the focal neurological alteration of sudden onset, where the patient may even be talking and suddenly show loss of muscle strength on one side of the body, dysarthria, even drowsiness.
Seizures may be present, but they are rare.
The neurological deterioration is progressive, which can be aggravated after 30 minutes or 1 hour after the event.
Signs of Cranial Endo Hypertension, such as headache (headache) and vomiting in the form of a projectile, may be present.
The most frequent hypertensive hemorrhage is that found in the putamen, followed by the adjacent internal capsule. And it is for this reason that on physical examination we observe contralateral hemiplegia.
When the hemorrhage is abundant, the drowsiness progresses to stupor and even coma, which can compromise the respiratory pattern. Accompanied by ipsilateral mydriatic pupil (dilated pupil) and fixed, bilateral positive Babinski signs and meningeal signs such as neck stiffness.
Thalamic hemorrhages also cause hemiplegia or hemiparesis as a result of compression or dissection of the adjacent internal capsule.
On many occasions the patient manifests a pronounced sensory deficiency that encompasses all modalities of sensitivity. For example, when hemorrhage is located in the dominant (left) thalamus it is accompanied by aphasia, often retaining verbal repetition, as well as apractognosia or mutism.
Other times a defect of the whole visual field tends to show a deviation of the eyes downwards and inwards, therefore, they have a peculiar way of looking at the nose; anisocoria with absence of light reflexes; oblique deviation with the contralateral eye to the hemorrhage displaced downwards and inwards.
Hemorrhages at the level of protrusion are manifested with tetraplegia over several minutes, with rapid and progressive deterioration of their neurological status, observing punctiform pupils with photomotor reflex, as well as hyperpnea, severe hypertension and hyperhidrosis. Death ensues after a few hours, this type of injury has a very poor prognosis.
The cerebellar hemorrhages evolve over several hours and are manifested by a picture of occipital headache, nausea, vomiting, dizziness and gait ataxia. It is often accompanied by paresis of the conjugate lateral gaze towards the side of the hemorrhage, forced deviation of the eyes towards the opposite side or paralysis of the sixth ipsilateral cranial nerve.
Other ocular signs that are infrequent are blepharospasm, which consists of the involuntary closing of an eye, eye jerking and very peculiar oblique deviation. it also produces dysarthria and dysphagia. With the passing of the hours, the patient may present a picture of stupor followed by coma by compression of the brainstem or by obstructive hydrocephalus.
Immediate surgical evacuation of the hemorrhage before compression of the brainstem occurs saves the patient's life.
Diagnostic
Cranial tomography and brain magnetic resonance continue to be the methods of choice for the initial diagnosis of intraparenchymal hemorrhage.
The images of blood flow in the MRI allow to identify the presence of arteriovenous malformations as a cause of the hemorrhage.
MRI angiography and conventional CT angiography by X-ray are performed when the cause of intracranial hemorrhage is unclear, especially when the patient is not hypertensive and the hematoma is not located in any of the four usual areas of hypertensive hemorrhage . For example, a hemorrhage in the temporal lobe suggests the rupture of a saccular aneurysm of the middle cerebral artery.
In these cases the use of lumbar puncture is never recommended because of the high risk of triggering a brain herniation.
Courtesy of Dr. Ana Estrada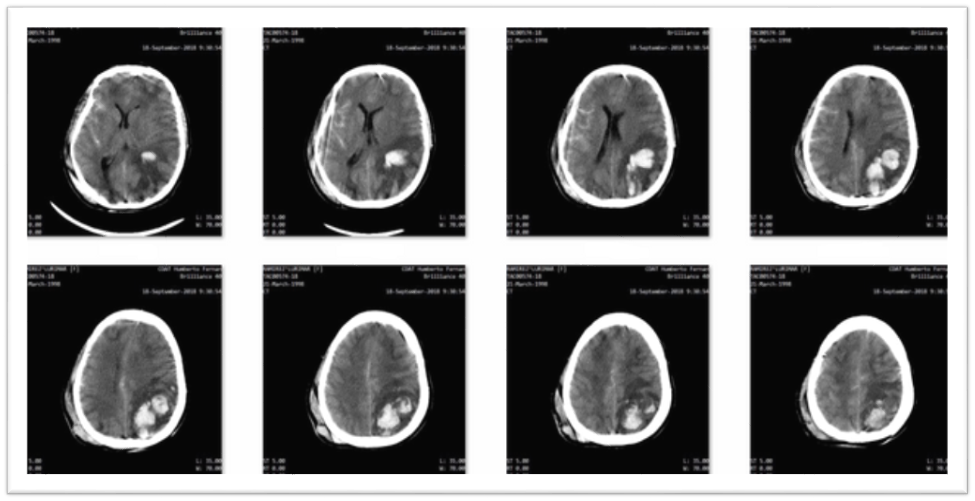
Images courtesy of anestrada12
Forecast
50% of patients with hypertensive intracerebral hemorrhage die, but there are cases where they can recover fairly well or even completely, which happens in cases where the bleeding is mild and there is no significant neurological damage.
We must bear in mind that the volume and location of the hematoma are the factors that govern the prognosis. In general terms, hematomas containing less than 30 ml of blood have a good prognosis, while those of 30 to 60 ml are of intermediate prognosis and the hematoma containing more than 60 ml has an initial gloomy prognosis.
The extension into the ventricular system worsens the prognosis. And more so in patients receiving anticoagulation in a therapist-based pathology, for example, atrial fibrillation.
Treatment
Initially, if the patient is under the context of intraparenchymal hemorrhage with high blood pressure figures, the first thing we must do is normalize the tension figures in the first 48 hours, give life support measures in severe cases, oxygen, parenteral electrolyte hydration , use of antibiotic therapy. In case of active infectious focus, for example if the patient during the cerebrovascular event bronco-aspiration and what is known as broncho-aspiration pneumonia occurs.
The evacuation of the hematoma is not usually useful, with the exception of cerebellar hemorrhages. In this type of hemorrhage, a neurosurgeon should be consulted to participate in the assessment of the patient; most cerebellar hematomas more than 3 cm in diameter require surgical evacuation.
Patients with a hematoma of 1 to 3 cm should be kept under observation to detect any data that indicate alterations of consciousness, which usually indicate that surgery is necessary.
Medical treatment during the acute phase of the cerebral hematoma helps to achieve a considerable recovery.
Prevention
Hypertension is the main cause of primary cerebral hemorrhage, it is for this reason the adequate control of it decreases the incidence rate of these fatal cases. Therefore, prevention should be directed towards the control of hypertension.
The reduction in the consumption of alcohol and other drugs such as cocaine and amphetamines.
Sources of support in the publication
- Update in Intracerebral Hemorrhage. Neurohospitalist. 2011 Jul; 1(3): 148–159.
- CT Protocol for Acute Stroke: Tips and Tricks for General Radiologists
- Neuroimaging of Hemorrhage and Vascular Defects. Neurotherapeutics. 2011 Jan; 8(1): 28–38.
- Vascular Neuro-ophthalmology. Handb Clin Neurol. Author manuscript; available in PMC 2010 Dec 6.
- Learn more about Posterior Cerebral Artery/Stroke II Geraint Fuller MA MD FRCP, Mark Manford BSc MBBS MD FRCP, in Neurology (Third Edition), 2010
- Internal carotid artery
- Head injury
- Clinical and radiological features of intracerebral haemorrhage in hypertensive patients. J Pak Med Assoc. 2008 Jul;58(7):356-8.
- Imaging of Intracranial Hemorrhage. J Stroke. 2017 Jan; 19(1): 11–27.
- Stroke Imaging
- Emergency neurological care of strokes and bleeds. J Emerg Trauma Shock. 2010 Jan-Mar; 3(1): 52–61.
- The Effects of Alcohol and Drugs of Abuse on Maternal Nutritional Profile during Pregnancy. Nutrients. 2018 Aug; 10(8): 1008.
- Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) II: Design, Methods, and Rationale. Neurocrit Care. Author manuscript; available in PMC 2012 Dec 1.
- Intraparenchymal hemorrhage
- Spontaneous intracerebral hemorrhage: a review. Matthew E. Fewel, B. Gregory Thompson Jr. and Julian T. Hoff
- Hydrocephalus
- Introduction to Pupillary Responses
- Hemorrhagic Stroke
- Computed tomography angiography or magnetic resonanceangiography for detection of intracranial vascularmalformations in patients with intracerebral haemorrhage(Review). CochraneDatabase of Systematic Reviews. Josephson CB, White PM, Krishan A, Al-Shahi Salman R.
- Neuroimaging in Intracerebral Hemorrhage
-

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
I hope you enjoyed my content.
Originally posted here: https://steemit.com/steemstem/@anaestrada12/intraparenchymal-hem-1556157441

No comments:
Post a Comment