This represents one of the most common neurological disorders in the world, with a high mortality and disability rate. Two etiologies are described: Ischemic and Hemorrhagic. Of which for the next post we will develop the one of ischemic origin.
Its frequency increases with age and associated comorbidities, such as high blood pressure, diabetes mellitus, obesity, arteromatous disease of great vessels, among others.
Almost all cerebrovascular diseases are characterized by a focal neurological deficiency of sudden and sudden onset, expressed in hemiparesis, alteration of cranial pairs, and dysarthria. For this reason, its diagnosis is clinical and we reinforce it with neuroimaging studies.
We must bear in mind that the clinical manifestations of stroke are very variable, and this is a consequence of the anatomical complexity of our Nervous System.
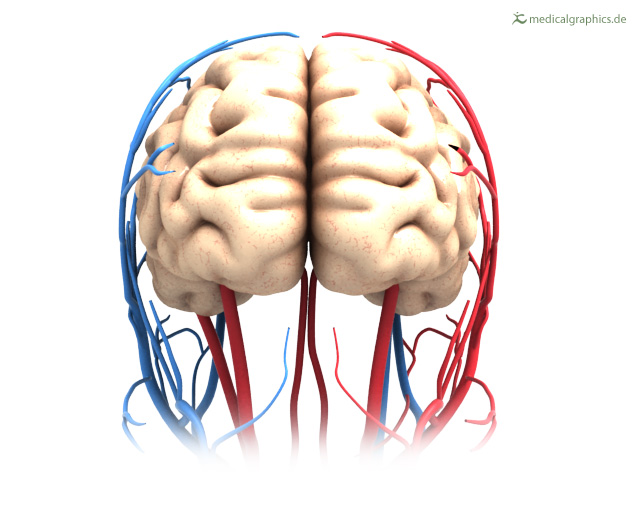
medicalgraphics.de. Public domain image

Brain vascular ischemic event presentation
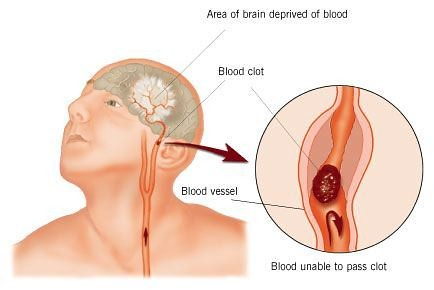
Cerebral ischemia is caused by reduced blood flow for a few seconds, thus symptoms appear in seconds by neuronal deprivation of glucose.
When the irrigation is restored in a short time the neuronal tissue recovers completely and the symptoms will only be transitory:
- This is what is known as a transient ischemic attack (TIA). The signs and symptoms of TIA last approximately 5 to 15 minutes and never exceed 24 hours.
- When the irrigation is interrupted for a longer time the result is an infarct or death of the affected encephalic tissue or what is called cerebrovascular disease of ischemic etiology and it is for this reason that we can observe the symptoms for more than 24 hours.
-
Cerebral hypoperfusion secondary to hypotension such as arrhythmias, acute myocardial infarction or hypovolemic shock triggers syncope (loss of consciousness for less than 5 minutes). If this deficit persists, the so-called cerebral infarcts appear in the bordering zones, taking the great arteries that irrigate the brain, affecting more frequently the middle cerebral artery, they are generally extensive lesions.
On the other hand, there is ischemia or focal infarction, which are the product of thrombosis of the cerebral vessels or by emboli that originate from an artery close to the heart.

Physiopathology
Sudden occlusion of an intracranial vessel reduces the blood flow in the encephalic region that the vessel irrigates, therefore the clinical consequences will depend on the irrigation of that artery.
The complete obstruction of cerebral circulation causes the death of the cerebral tissue within 4 to 10 minutes. If the bloodstream is resumed before a large number of cells have died, the individual experiences transient symptoms, such as a transient ischemic attack.
There is an ischemic penumbra, which represents the tissue surrounding the ischemic zone, and if dysfunction can be reversible. Of course, if there are no changes in the irrigation, as soon as possible the ischemic penumbra will culminate in a heart attack and for this reason the importance of its diagnosis by means of neuro-imaging and early initiation of treatment.
Cerebrovascular accident. Public domain image. Source FlickrCells usually die through two routes:
- Necrosis, where degradation of the cellular cytoskeleton is rapid, due to the absence of energetic substrates.
- Apoptosis, where the cell is "programmed" to die.
-
In a simple way, ischemia produces necrosis by depriving neurons of glucose, thus preventing the production of adenosine triphosphate (ATP) in the mitochondria and thus their death.

Clinical Case Report
Female patient of 24 years of age, with obstetrical antecedents of an abortion 2 years ago, who according to presents clinical neurological focus after segmental caesarean section, presenting loss of muscle strength of right hemi-body accompanied by dysarthria of abrupt presentation reason for which they request evaluation by internal medicine service.
Personal history
- Denies DM, HTA, asthma, drug allergy.
- Surgical interventions; recent segmental caesarean section.
- Appendectomy at age 17 without complications.
- G.O.: II pregnancies.
- I Cesarean section. I Abortion.
- Menarche 14 years old. Eumenorheic.
-
Family history
- Mother: apparently healthy.
- Father: Seemingly healthy.
- Son: 1 Apparently healthy.
- Maternal Cousin: history of Systemic Lupus Erythematosus.
-
Habits
Denies consumption of alcoholic beverages and tobacco. Refers coffee consumption 2 cups a day.
Physical Exam
- Blood pressure: 110/ 80 mmHg.
- Heart rate: 78 Lpm.
- Respiratory frequency 18Rpm.
- Oxygen saturation: 97% ambient air.
-
Patient in stable conditions afebrile to the touch, eupneic hydrated, light paleness cutaneous mucous, tolerating oxygen environment. Pupils isocoric normo reactive to light, oral cavity without alterations, painless mobile neck, thyroid not palpable, carotid pulse present of good intensity without adenopathies. Chest symmetrical turgid breasts, painful on palpation and with exit of secretion type breastfeeding, apex in 5 to intercostal space CML, rhythmic heart sounds without murmur. Audible respiratory noises in both pulmonary fields without aggregates. Soft depressible abdomen, no pain RsHsAs present, no visceromegaly, no signs of peritoneal irritation. Symmetrical extremities without edema, peripheral pulses present. Neurological: vigil, consciously oriented in time, space and person. Dysartric language. Impression 7th right central cranial nerve. Right hemiparesis FM I/V, without meningeal signs.
Laboratory tests
CB 11.000 Sec 78% Lymphocytes 32% Bilirrubin 1.1 Plaq 130,000 Urea 19 Cholesterol 170 Creatinine 0.7 Triglycerides 100 TGO 28 TGP 31 Uroanalysis:
- Physical Analysis: Intense Yellow; Ph 6.5; Acid reaction, cloudy appearance, Density 1020.
- Chemical analysis: Ketone (-), urobilinogen (-), hemoglobin ++, trace proteins, nitrites +.
- Microscopic analysis: Leukocytes 18 to 20 xc, epithelial cells 1-3 xc, abundant bacteria, red blood cells 10 to 15xc.
-
Doppler carotid basilar vertebral ultrasound: No hemodynamic repercussion.
Abdominal- pelvic ultrasound: only a simple cyst of the left ovary is reported.

Magnetic Resonance

@anestrada12 Cut at T2: Ischemic lesion in left hemisphere of parieto-occipital location is evident.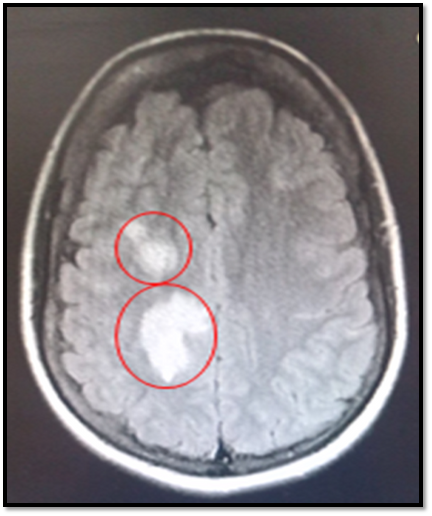
@anestrada12. In diffusion, where ischemia stands out and shines, they are suggestive signs of an acute event of ischemic etiology.
@anestrada12. Coronal Cut T1 shows hypointensity lesions suggestive of ischemia in the left hemisphere.
Conclusions
Brain vascular events are not common in young patients, they are generally characteristic of patients with advanced age and certain comorbidities, such as diabetes mellitus, arterial hypertension, cardiac arrhythmias among others, and when this neurological pathology becomes present in young people, it is to be thought that possibly an immunological disease is implicated that predisposes to the appearance of the same, such is the case of the Antiphospholipidic Syndrome and the Systemic Lupus Erythematosus.
Antiphospholipidic syndrome is understood as that immunological pathology that generates a state of hypercoagulability, capable of triggering episodes of arterial and/or venous thromboembolism, usually accompanied by recurrent fetal losses, thrombocytopenia and specific elevated antibodies.
The clinical manifestations in this syndrome are multiple and diverse, depending on the branch of artery or venous affected and therefore the system that irrigates will give us the corresponding clinic, as is the case of DVT in lower limbs, vascular brain events, superficial thrombophlebitis, ulcers more frequently in legs that can become complicated with cutaneous necrosis, subungual hemorrhages, purpuric lesions and pseudovasculitis.
The diagnosis of this immunological disease is given by means of Serologies for specific antibodies; Anticarliodipine Antibody IgM or IgG, Lupus Anticoagulant, and Anti ß2 glycoprotein 1.
While Systemic Lupus Erythematosus, a chronic and inflammatory autoimmune disorder, where the body's own antibodies mistakenly attack healthy tissue, such is the case of the skin, kidneys, joints, brain among others. It most often affects the female sex, having a peak incidence in the 2 and 3 decade of life.
Currently, our patient is waiting for results in the serology of Antiphospholipidic Syndrome and Systematic Lupus Erythematosus. With the following diagnoses: Left Ischemic Cerebrovascular Event. For which it receives treatment with an antiplatelet type Clopidrogel 75mg V.O OD.
Sources of support in the publication
- Case Studies in Stroke - Common and Uncommon Presentations
- Cerebrovascular Diseases
- Brain Stem Stroke
- Signals and signs in the nervous system: The dynamic anatomy of electrical activity is probably information-rich
- Cerebral vascular dysregulation in the ischemic brain
- Brain ischemia
- Transient ischemic attack
- Diagnosis and Management of Transient Ischemic Attack
- What you need to know about cerebrovascular disease
- The Comprehensive Stroke Center at University Hospital Types of Stroke
- Transient ischaemic attack (TIA)
- Brain ion homeostasis in cerebral ischemia
- Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018
-

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
I hope you enjoyed my content.
Originally posted here: https://steemit.com/steemstem/@anaestrada12/let-us-know-a-little-1559527051
No comments:
Post a Comment